
Before the beginning of 2018, when I was experiencing the onset of hypertension, diabetes, anal fissure, and tooth cavities, magic happened.
For no reason, I heard about conscious eating in the holistic sessions of any organization on television. I explored more videos on holistic conscious eating.
That changed my life. I started eating mindfully, focused on food vibrations and affirmations, and in three months my hyperglycemic readings were changed, hypertension medicines were stopped, and I never needed surgical interventions for anal fissures.
What is conscious eating?
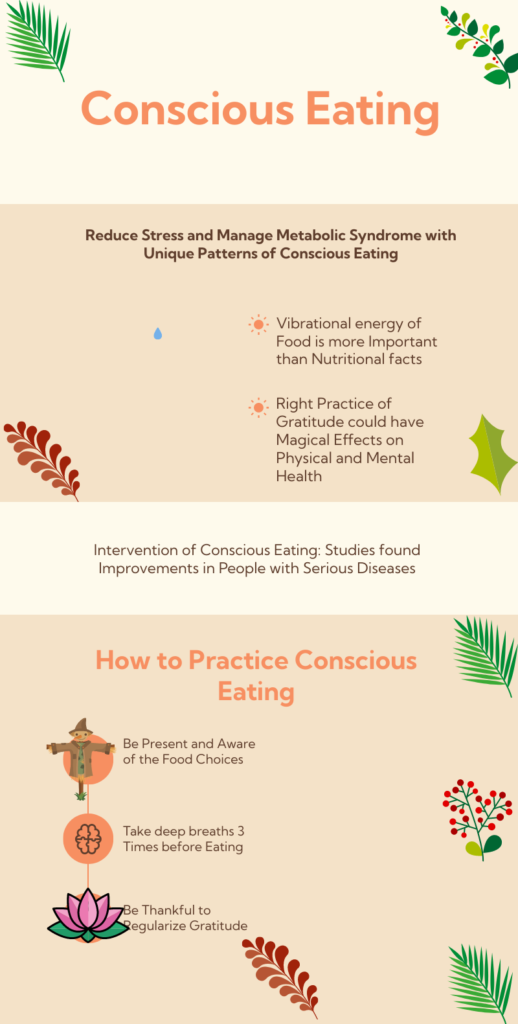
Conscious eating is the right way of eating to integrate your presence and attention toward food. Mindful eating has the potential to reduce stress and manage metabolic syndrome. Listen to what your body signals to acknowledge all senses and learn the engaging benefits of conscious eating.
No need to focus on each what and why of eating
Focusing on nutritional fact checks, calorie checks, and additional values of each food material could trigger psychological barriers. These practices could leave the person with more comorbidities due to psycho-emotional priorities in the wrong direction. For example, anorexics always think about food and food-related perceptions, resulting in mental and behavioral complexities.
Listen to engaging senses to reduce stress and manage metabolic syndrome.
Five engaging senses include sight, sound, taste, smell, and touch. Focusing on these senses promotes physical and mental relaxation to prevent overthinking and thought barriers. Also, sensory engagement with conscious eating reduces stress by activating pleasure harmones. For example, a person diagnosed with Cushing’s syndrome should try the methods of mindful eating to experience magical effects.
Be present with conscious eating to reduce stress
In a world of endless distractions and hurried meals, the 3 R’s of mindful eating—Reduce, Reconnect, and Relish—invite us to transform nourishment into a sacred act of presence.
Reducing does not mean decreasing your meal which could alter body functions and alleviate stress. It urges us to slow down, silencing the chaos around us: chew deliberately, set down utensils between bites, and tune into hunger cues rather than autopilot consumption.
Reconnect bridges the gap between plate and planet, asking us to honor the journey of our food—the soil, hands, and processes that brought it to our table—cultivating gratitude and ecological awareness. Gratitude toward everything reduces stress and manages metabolic syndrome.
Finally, Relish is the art of reflecting the awakening senses physically and emotionally often numbed by screens and routines. Together, these R’s don’t just combat overeating—they rewire our relationship with food, turning meals into meditations that nourish body, mind, and soul. By embracing this triad, we don’t just eat; we feast on the poetry of being alive.
Food Vibrations: Beyond Nutrition
Some holistic traditions propose that foods carry energetic “vibrations,” influenced by freshness, sourcing, and preparation. While this concept is metaphysical rather than scientifically validated, it encourages prioritizing whole, minimally processed foods:
- High-Vibration Foods: Fresh fruits, vegetables, leafy greens, nuts, seeds, sprouted grains, and herbs. These are often linked to vitality and clarity.
- Lower-Vibration Foods: Highly processed items, artificial additives, alcohol, and caffeine. Some traditions also classify non-vegetarian foods as lower vibration due to ethical or energetic concerns, though nutritional science emphasizes balance and personal choice.
Note: Regardless of dietary preferences (plant-based or omnivorous), focus on ethically sourced, high-quality ingredients to align with conscious eating principles.
The Power of Choice
Every meal is an opportunity to make intentional decisions:
- Align with Values: Choose foods that reflect your health goals, ethics, and environmental awareness.
- Mindful Selection: Ask, “Does this food nourish my body and uplift my spirit?”
- Break Autopilot: Replace impulsive eating with pauses to check in with hunger cues and emotions.
Daily Affirmations for Mindful Eating
Affirmations reinforce positive attitudes and behaviors. Examples:
- “I choose foods that honor my body’s wisdom.”
- “I eat with gratitude, joy, and presence.”
- “Every bite connects me to vibrant health.”
Science of Affirmations
- Self-Affirmation Theory: Affirmations activate brain regions linked to self-worth (ventromedial prefrontal cortex), reducing stress and improving decision-making.
- Neuroplasticity: Repetition rewires neural pathways, fostering resilience against emotional eating.
- Behavioral Reinforcement: Positive statements boost self-efficacy, making healthier choices feel more achievable.
Conscious Eating to Reduce Stress
Mindful eating lowers stress by:
- Slowing Down: Chewing thoroughly and savoring meals reduces cortisol (stress hormone) levels.
- Engaging Senses: Focus on colors, textures, and aromas to anchor in the present moment.
- Releasing Judgment: Replace guilt with curiosity about how foods make you feel.
Reversing Metabolic Syndrome
Studies suggest mindful eating can improve metabolic health by:
- Reducing Overeating: Tuning into satiety cues prevents excess calorie intake.
- Balancing Blood Sugar: Prioritizing fiber-rich, whole foods stabilize glucose levels.
- Combating Inflammation: Antioxidant-rich, high-vibration foods (e.g., berries, leafy greens) mitigate oxidative stress linked to metabolic disorders.
Practical Steps to Start
- Begin with Breath: Take 3 deep breaths before eating to center yourself.
- Gratitude Ritual: Acknowledge the journey of your food from source to plate.
- Affirmation Integration: Pair meals with a mantra to reinforce intentionality.
How Conscious Eating Lowers Hypertension Risk?
Hypertension, a leading risk factor for heart disease, is closely tied to dietary habits and lifestyle. Conscious eating—a mindful approach to food—emerges as a powerful tool to combat high blood pressure while addressing broader health challenges like metabolic syndrome and stress.
Manage Metabolic Syndrome Through Mindful Choices
Metabolic syndrome, a cluster of conditions including hypertension, high blood sugar, and excess abdominal fat, thrives on poor dietary patterns.
Conscious eating encourages nutrient-dense, whole foods over processed options, by limiting the options of sodium and sugary diet. By fostering portion awareness and balanced meals (rich in fiber, potassium, and healthy fats), this practice helps regulate blood pressure, stabilize blood sugar, and support weight management—key steps in managing metabolic syndrome.
Reduce Stress to Protect Your Heart
Stress triggers cortisol release, which elevates blood pressure and drives unhealthy eating habits. Conscious eating interrupts this cycle by transforming meals into moments of calm.
Focusing on the sensory experience of eating—savoring flavors, and chewing slowly—activates the body’s relaxation response, lowering cortisol levels. Over time, this reduces stress-induced hypertension and curbs emotional eating, promoting metabolic resilience.
Moreover, conscious eating focuses on the concept of gratitude that discourages negative thoughts. Gratitude is a powerful tool to balance physical and mental health with reduced stress and patterns of overthinking. Finally, managing metabolic syndrome like hypertension is feasible without medication adherence.
Begin with these steps:
- Eat without distractions (avoid screens or multitasking).
- Listen to hunger cues—pause to assess fullness.
- Choose whole foods like leafy greens, berries, and nuts.
- Breathe deeply before meals to center yourself.
By merging mindful food choices with stress reduction, conscious eating offers a holistic path to lower hypertension risk and enhance overall well-being. Small shifts in how we eat can yield profound impacts on heart health and metabolic vitality.
Case Study: Survival Beyond 14 Years Post-Hypertensive Crisis Through Lifestyle Modifications
Patient Presentation
Name: John Doe (pseudonym)
Age: 52 years
Gender: Male
Medical History: Obesity (BMI 32), sedentary lifestyle, poorly controlled hypertension, metabolic syndrome (elevated fasting glucose, dyslipidemia).
Initial Presentation:
Mr. Doe presented to the emergency department with a hypertensive crisis (BP 210/120 mmHg), complaining of severe headache and dizziness. Initial evaluation (ECG, troponin, creatinine, urinalysis, fundoscopy) revealed no end-organ damage, classifying this as a hypertensive urgency. He was stabilized with IV antihypertensives (labetalol) and discharged with oral amlodipine, lifestyle modification advice, and a 7-day follow-up.
Clinical Course Over 1 Month
- Week 1-2 Post-Discharge:
- Mr. Doe resumed poor dietary habits (high sodium, processed foods) and ignored follow-up appointments.
- Stressors: High work-related stress and sleep deprivation.
Week 3-4:
- Readmitted with pneumonia (fever, hypoxia) requiring antibiotics and oxygen therapy.
- Developed acute cardiorenal complications:
- Cardiovascular insufficiency: Elevated NT-proBNP, reduced ejection fraction (45%).
- Acute kidney injury (AKI): Creatinine 2.4 mg/dL (baseline 1.1 mg/dL).
- Hospitalized for 4 weeks with multidisciplinary care (cardiology, nephrology, critical care).
Post-Hospitalization Interventions
- Conscious Eating:
- Adopted a plant-based, low-sodium diet with portion control and mindful chewing.
- Focused on whole foods (fiber-rich vegetables, omega-3 sources) to manage metabolic syndrome.
- Stress Reduction:
- Integrated daily meditation and diaphragmatic breathing exercises.
- Transitioned to a less stressful job and prioritized sleep hygiene.
- Medical Management:
- Optimized antihypertensives (ACE inhibitor + thiazide diuretic).
- Statins for dyslipidemia and metformin for insulin resistance.
- Physical Activity:
- Gradual introduction of walking (30 mins/day), progressing to light resistance training.
Outcome
- 1-Year Follow-Up: BP stabilized to 130/85 mmHg; creatinine normalized (1.2 mg/dL); LDL-C <100 mg/dL.
- 5-Year Follow-Up: No recurrent hospitalizations; resolved metabolic syndrome (BMI 28, HbA1c 5.7%).
- 14+ Years Post-Crisis: Lived independently until age 66, with eventual death due to unrelated causes (trauma).
Discussion
Mr. Doe’s survival beyond 14 years (exceeding the 55% 5-year survival rate post-hypertensive crisis) highlights:
- Conscious Eating: Reduced sodium and calorie intake improved BP control and reversed metabolic syndrome.
- Stress Reduction: Lower cortisol levels mitigated sympathetic overdrive, protecting cardiovascular and renal function.
- Metabolic Syndrome Management: Addressing insulin resistance and dyslipidemia prevented secondary organ damage.
Key Takeaway: Integrative lifestyle changes (diet, stress, activity) synergize with pharmacotherapy to enhance longevity in high-risk patients. John Doe practiced the insights of mindful eating with each meal, and every sip of water, and survived longer than expected.
Clinical Implications
- Preventive Focus: Post-crisis care must emphasize patient education on lifestyle modifications.
- Multidisciplinary Approach: Collaboration between dietitians, mental health professionals, and physicians improves outcomes.
Can conscious eating rituals reduce stress?
Conscious Eating Rituals and Stress Reduction: The Role of Cortisol and Metabolic Syndrome Management
Cortisol, Stress, and Eating
Cortisol, the primary stress hormone, spikes during stress, triggering “fight or flight” responses. Chronically elevated cortisol is linked to overeating, abdominal fat accumulation, insulin resistance, and hypertension—key factors in metabolic syndrome (a cluster of conditions including high blood sugar, obesity, and dyslipidemia)
How Conscious Eating Lowers Cortisol?
- Parasympathetic Activation: Mindful eating shifts the body to “rest and digest” mode, reducing cortisol production.
- Reduced Emotional Eating: Addressing stress-driven cravings, prevents cortisol spikes from sugary/fatty foods.
- Improved Meal Rhythm: Slower eating aids digestion and stabilizes blood sugar, indirectly lowering stress.
Link to Metabolic Syndrome Management
Lower cortisol levels from mindful eating can:
- Improve Insulin Sensitivity: Reducing stress-related glucose spikes.
- Promote Healthy Weight: Mitigating cortisol-induced abdominal fat storage.
- Lower Blood Pressure: Stress reduction supports cardiovascular health.
Real-Time Examples
- University Study: A 2016 study (e.g., Journal of Obesity) found obese adults practicing mindful eating for 12 weeks had lower cortisol levels, reduced waist circumference, and improved HbA1c.
- Workplace Wellness Programs: Companies like Google integrate mindful eating workshops, reporting reduced employee stress and fewer midday energy crashes.
- Individual Practice: A person practicing a “5 senses check” before meals (noticing food’s color, smell, and texture) reports less stress and better portion control, aiding weight management.
Practical Rituals to Try
- Pre-Meal Breathing: Take 3 deep breaths to activate relaxation.
- Tech-Free Meals: Eliminate screens to focus on eating.
- Gratitude Integration: Be thankful for every sense of food before eating to soothe the deeper insights.
Pingback: Cancer Due to Stress: Break the Cycle! Revolutionary Tactics to Prevent Recurrence and Reclaim Your Health - thoughtbooster.org
Pingback: 5 Best Suggested Protein Supplements to Advocate ICMR Guidelines - thoughtbooster.org