Is Chronic Stress the Major Contributor of Cancer Relapse?

What is Chronic Stress?
Researchers are curious to break the psychology of cancer due to stress. Short-term stress induces physical and mental health issues for a short period. Depending on the response to the particular events, it may last weeks or months.
Chronic stress is the long-term prevalence of stress related to work pressure, financial difficulties, academic failure, etc. Chronic stressors are at an increased risk of metabolic disorders, heart diseases, and debilitating immune systems.
What is cancer Recurrence?
With combined strategies of chemotherapy, surgery, radiation, and holistic measures, cancer is treated. Once treated, some of the cancer cells survive even with the completion of the treatment procedure. These cancer cells flourish over time and grow in different body locations. Cancer relapse may be local (growth of malignant tumor in the same location), regional (relapse of malignant tissues in the lymph nodes), and distant (growth of tumor in other location leaving original).
Chronic Stress and Cancer Recurrence: Unraveling the Invisible Thread
The relationship between chronic stress and cancer recurrence has long intrigued researchers, with mounting evidence suggesting that psychological distress may act as a silent catalyst for disease progression. While cancer treatment has advanced significantly, the role of stress physiology—particularly in vulnerable patients—remains a critical, yet underexplored, factor in relapse. This article examines the biological interplay between cancer due to stress and cancer recurrence, illustrated through a poignant case study, and explores strategies to mitigate this risk.
Stress Physiology in Cancer Patients
Newly diagnosed cancer patients often experience a surge in stress hormones due to the activation of the hypothalamic-pituitary-adrenal (HPA) axis and sympathetic nervous system (SNS). Cortisol and adrenaline, the primary stress hormones, suppress immune function by reducing natural killer (NK) cell activity—a frontline defense against cancer cells. Simultaneously, chronic inflammation, driven by cytokines like IL-6 and TNF-alpha, creates a microenvironment conducive to tumor growth and metastasis. For patients undergoing chemotherapy or radiation, this dual burden of treatment-induced physical stress and psychological strain may inadvertently fuel residual cancer cells.
Case Study: Mervlyn’s Journey (2015–2022)
Diagnosis & Initial Treatment (2015):
At 42, Mervlyn was diagnosed with stage II hormone receptor-positive breast cancer. She underwent a lumpectomy, followed by adjuvant chemotherapy and radiation. Her oncology team emphasized holistic care: mindfulness meditation, a plant-based diet, and yoga to manage treatment side effects and stress. For three years, Mervlyn remained in remission, attributing her resilience to this integrative approach.
Day-to-Day Stressed Journey of a Single Mother with Breast Cancer Recurrence
6:00 AM:
Her alarm blares, but she’s already awake, haunted by a nightmare of scans and suffocating medical bills. Fatigue clings to her bones, a remnant of yesterday’s chemotherapy. She swallows nausea pills, then tiptoes to the kitchen, calculating the cost of groceries and medical bills.
She is making breakfast with constant negative thoughts of death and dying, financial burdens, education of children, and so on.
7:30 AM:
The kids—Lily, 8, and Jake, 10—stumble into the kitchen. She masks her shaking hands with a smile, brushing off Lily’s worried stare. “Mom’s just tired, sweetheart.” Her phone buzzes: a reminder for her 10 AM conference call. Work expects her to present a project update, but her brain feels fogged, words slipping like sand. She cancels Jake’s dentist appointment—another $150 saved—and swallows guilt with her coffee.
9:00 AM:
At the infusion center, she texts her boss: “Working remotely today—minor appointment.” The lie burns. Her laptop balances on her knees as the IV drips. A coworker pings: “Need those numbers ASAP.” She types one-handed, her free arm stiffening from the needle. The nurse mentions a new drug not covered by insurance. Her stomach knots—$1,200 a dose.
2:00 PM:
Home between Zoom meetings, she scrambles to fold laundry and prep dinner (frozen pizza—again). A bill collector calls. “Payment overdue.” She hangs up, tears pricking her eyes. Jake asks for help with math homework. Her hands tremble as she solves equations, her mind flashing to the PET scan next week. What if it’s spread? Who’ll care for them? Was the cancer growing due to stress?
6:30 PM:
Dinner is silent except for the kids’ chatter. Lily draws a picture of “Super Mom” in a cape. The lump in her throat grows. She excuses herself to vomit, the chemo raging. Jake knocks: “Mom? You okay?” She rinses her mouth and straightens her shirt. “Just a bug, honey.”
9:00 PM:
The kids are asleep. She opens her laptop, chasing deadlines. Her boss emails: “Missed targets this month. Let’s discuss tomorrow.” Panic claws her chest. She downs a painkiller, fingers hovering over a GoFundMe page—“Single Mom Fighting Cancer Round 2.” Pride stalls her. The fridge hums. The clock ticks.
11:30 PM:
In bed, her mind races. Relapse stats. Job loss. Mortgage. Funeral costs. She grips her chest, phantom pain mirroring her fear. A muffled cry escapes—grief for the future she’d rebuilt, now crumbling. But she stifles it. The kids need her. Always.
Cycle repeats.
Themes:
- Financial Pressure: Choosing between treatment and groceries, debt collectors, rationing resources.
- Work Pressure: Juggling deadlines and chemo, fear of job loss, masking pain to stay employable.
- Relapse Thoughts: Intrusive “what-ifs,” guilt over mortality, the terror of leaving her children.
Emotional Undercurrents:
A relentless tug-of-war between survival and surrender. Moments of raw vulnerability punctured by forced strength. Love for her children as both anchor and weight. The cruel irony of beating cancer once, only to face it again—weaker, poorer, lonelier. Yet, each dawn, she rises. Not for hope, but for them.
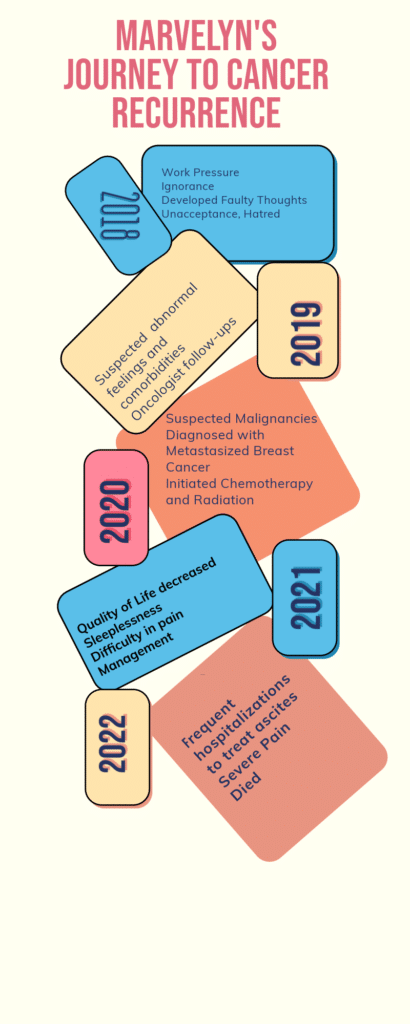
Relapse (2018):
Life took a devastating turn in 2018. As a single mother after her husband’s sudden death, Mervlyn faced overwhelming work pressure and financial strain. Her cortisol levels spiked, her sleep deteriorated, and she abandoned stress-management practices. Within months, she noticed unexplained weight loss and fatigue. Imaging revealed metastatic breast cancer in her bones and liver.
Final Years (2019–2022):
Mervlyn’s cancer progressed rapidly despite endocrine therapy and targeted treatments. The liver failure led to debilitating ascites, requiring weekly paracentesis. Though palliative care improved her quality of life, she passed away in 2022, underscoring the grim trajectory of stress-exacerbated disease.
Stress Modulators: How Stress Fuels Relapse
Chronic stress amplifies cancer risk through several pathways:
- Hormonal Dysregulation: Elevated cortisol and norepinephrine promote angiogenesis and cancer cell migration via β-adrenergic signaling.
- Immune Suppression: Reduced NK cell activity allows dormant cancer cells to evade detection.
- Epigenetic Changes: Stress-induced glucocorticoids may alter gene expression, activating oncogenes.
Studies corroborate this link. A 2020 Nature Reviews Cancer analysis highlighted that stress neurotransmitters accelerate metastasis in breast and ovarian cancers. Similarly, a longitudinal study in Cancer Research (2019) found that breast cancer survivors with high perceived stress had a 45% higher recurrence risk over five years.
Holistic Strategies to Prevent Recurrence
To disrupt this cycle, integrative approaches are vital:
- Pharmacological: Beta-blockers (e.g., propranolol) may inhibit adrenaline’s protumor effects.
- Psychological: Cognitive-behavioral therapy (CBT) and mindfulness reduce cortisol levels.
- Lifestyle: Regular exercise lowers inflammation, while social support buffers stress.
Research by Antoni et al. demonstrated that breast cancer patients in stress-management programs had lower inflammation markers and improved survival rates.
Conclusion
Mervlyn’s story mirrors a growing scientific consensus: chronic stress is not merely a bystander but a potent contributor to cancer recurrence. While it is seldom the sole factor, its synergy with biological vulnerabilities cannot be ignored. Empowering patients with stress-modulation tools—from therapy to community support—could redefine survivorship care, turning the tide against invisible triggers of disease.
“The mind is not a separate entity from the body,” Mervlyn once wrote in her journal. Her words remind us that healing demands addressing both.

Real-Time Case Stories when Cancer due to Stress occurred and Stress Management resulted in Miracles
Navjot Singh Sindhu was a former cricketer and politician in India. Recently, in 2024, his wife (Navjot Kaur Sindhu) won the battle against stage 4 cancer with lifestyle modifications. Though she underwent chemotherapy and surgery, her chances of survival were only 3% according to the best oncologists in the world. She survived a disciplined life.
What could be the disciplined life for a stage 4 cancer patient whose chances of survival are 3%?
Studies suggest she made dietary changes, focused on intermittent fasting, and adopted changes in lifestyle regimen. Dietary changes included apple cider vinegar, blueberries, gooseberries, lemon water, neem water, and other herbal remedies with the last meal at 6:30 in the evening and the first meal at 10:30 AM. She learned that cancer is due to stress and recurrence could be prevented by stress management.
Can everyone struggling with stage 4 cancer adopt this disciplined regimen?
No, but why? Comorbidities. Why comorbidities?
Again, the answer is a constant flow of negative thoughts related to unmanaged cortisol and adrenaline hormones in cancer patients prevents them from adopting healthy regimens. Cancer due to stress is the major cause of flourishing unhealthy cells in the body.
What is needed to reduce or prevent malicious growth in the body? Is it stress management?
While oncologists and other medical experts supported evidence-based chemotherapy and surgery for the treatment, survival cases of terminal cancers are rare.
Navjot Kaur trained her brain to think optimistically, which changed her subconscious mind patterns and influenced her coping mechanism. With a positive mindset, she actively adhered to medical treatments, avoided social withdrawal as most cancer patients prefer, and motivated psychological and emotional healing, with reduced onset of anxiety and depression.
Another story is from Sarcoma Oncology Center in 2010. Nancy Stordahl was diagnosed positive for BRCA2 mutation (a deadly breast cancer) with sudden onset of chest pain. With an advanced ultrasound, mammogram, and biopsy, her cancer was confirmed. In 2010, her treatment was started with a bilateral mastectomy. Further, chemotherapies followed by multiple side effects, genetic testing, and other biopsies were done.
She experienced various panic attacks related to stress, anxiety, emotional distress, and thoughts of death and dying. Later, she joined a support group for cancer patients where she revealed a life-changing experience to motivate her hopeful thoughts. Also, Nancy suggested that friends and family play a contributory role in changing the mental psyche of an individual.
Nancy’s cancer never returned since 2010 and till now she is a member of the cancer support group to help patients with emotional healing.
What is the Psyche behind Cancer and How to Prevent Cancer Recurrence?
Usually, when a patient is diagnosed or confirmed with cancer or cancer relapse, the first thought they create is of death and dying. Not limited to the patient, but the family members and friends start adjusting their thoughts to death and dying. Is it the belief system that kills the patient or induces a sudden peak of cortisol or adrenaline hormones among the vulnerable groups?
Can changing the belief system work?
Yes, of course. The patients who turned their deadly cancer cells into healthy tissues changed their belief systems. A change in belief system, whether positive or negative, has a direct impact on both physical and mental health. As such, negative beliefs about cancer could reduce the survival rate with low quality of life and painful death. Whereas, positive beliefs could foster resilience, a significant sense of control, improved health behaviors, and meaningful thoughts to turn the malicious cells down.
Role of Conscious Eating to Prevent Cancer Recurrence
Conscious eating is a mindfulness practice with powerful neural associations to treat structural and functional abnormalities in the brain. Cancer patients adopt this practice to surge cognitive balance and emotional motivations and control the flow of negative thoughts.
Studies found significant changes in neurotransmitters like dopamine (award and motivation hormones), serotonin (elevates mood and promotes sleep patterns), GABA, epinephrine, norepinephrine, and others with conscious eating. Also, altered neurotransmitters are related to the impaired gut-brain axis, negatively impacting the growth of bodily cells and debilitating digestion and immune functions.
Gut Microbiota, Stress, and Cancer: Mechanisms and Interventions
Microbiota Influencing Cancer Growth
Pro-Carcinogenic Microbes:
Fusobacterium Nucleatum: Linked to colorectal cancer (CRC) by promoting inflammation, activating oncogenic pathways (e.g., β-catenin), and suppressing immune responses.
Enterotoxigenic Bacteroides Fragilis (ETBF): Produces toxins that damage DNA and drive IL-17-dependent inflammation, increasing CRC risk.
Escherichia Coli (pks+ strains): Produce colibactin, a genotoxin causing DNA damage and mutations.
Streptococcus Gallolyticus: Associated with colorectal tumors and inflammatory bowel disease (IBD).
Microbes Reducing Cancer Risk:
- Lactobacillus spp., Bifidobacterium spp.: Produce short-chain fatty acids (SCFAs) like butyrate, which suppress inflammation, enhance gut barrier integrity, and induce apoptosis in cancer cells.
- Faecalibacterium Prausnitzii: Anti-inflammatory butyrate producer; low levels correlate with CRC.
- Akkermansia Muciniphila: Improves mucin layer integrity, reduces inflammation, and enhances immunotherapy efficacy.
- Roseburia spp.: Butyrate producers that modulate regulatory T-cells to suppress tumor growth.
Stress-Gut Microbiota Interactions
Chronic stress disrupts the gut-brain axis via:
- HPA Axis Activation: Cortisol release alters gut permeability (“leaky gut”), enabling bacterial translocation and systemic inflammation.
- Sympathetic Nervous System (SNS) Overdrive: Reduces gut motility and diversity, favoring pathobionts (e.g., Proteobacteria).
- Immune Dysregulation: Stress-induced cytokines (e.g., IL-6, TNF-α) promote a pro-tumor microenvironment.
- Microbial Metabolite Shifts: Stress depletes SCFA-producing bacteria, reducing anti-inflammatory signals.
Stress Modulators and Mechanisms
Psychobiotics: Probiotics (e.g., Lactobacillus Rhamnosus, Bifidobacterium Longum) modulate GABA and serotonin production, dampening HPA axis reactivity.
Mind-Body Therapies:
Mindfulness/Yoga: Lower cortisol and inflammation (reduced CRP/IL-6).
Cognitive Behavioral Therapy (CBT): Mitigates stress-induced dysbiosis.
- Pharmacological Agents:
- SSRIs/SNRIs: Increase BDNF, improving gut barrier function.
- Beta-Blockers: Counteract SNS effects on gut motility.
- Dietary Interventions:
- Prebiotics (e.g., inulin): Fuel-beneficial SCFA producers.
- Polyphenols (e.g., curcumin): Inhibit pro-inflammatory microbes.
Preventing Cancer Relapse & Managing Chronic Stress
Microbiota-Targeted Strategies:
Fecal Microbiota Transplantation (FMT): Restores eubiosis post-chemotherapy.
Personalized Probiotics: Tailored to replenish SCFA producers.
Stress Reduction Protocols:
Adaptogens (e.g., ashwagandha): Lower cortisol and stabilize the HPA axis.
Exercise: Increases microbial diversity (e.g., Akkermansia).
Integrated Care Models:
Combine immunotherapy with stress management (e.g., meditation) to enhance NK cell activity.
Monitor microbial biomarkers (e.g., F. Prausnitzii levels) in cancer survivors.
Key Takeaway: Stress-induced dysbiosis creates a pro-inflammatory, pro-tumor niche. Interventions targeting both microbiota (e.g., probiotics, diet) and stress pathways (e.g., mindfulness, adaptogens) synergistically reduce cancer risk and relapse.